Stage 2 Cervical Cancer: Symptoms, Diagnosis, and Treatment

Table of Contents
- What is Cervical Cancer?
- What is Stage 2 Cervical Cancer?
- Symptoms of Stage 2 Cervical Cancer
- Diagnosis of Stage 2 Cervical Cancer
- Treatment for Stage 2 Cervical Cancer
- Is Stage 2 Cervical Cancer Curable?
- Survival Rate of Stage 2 Cervical Cancer
- High-Risk Factors for Stage 2 Cervical Cancer
- Lifestyle Changes for Managing Stage 2 Cervical Cancer
- Does Stage 2 Cervical Cancer Affect Fertility?
- Word From An Expert
Did you know that cervical cancer is one of the most common cancers affecting women globally, yet it is highly preventable and treatable when detected early?
Let’s understand in detail about cervical cancer and what happens in its second stage.
If you are facing any health concerns, feel free to talk to the best doctors at Birla Fertility & IVF. Click here to book your appointment.
What is Cervical Cancer?
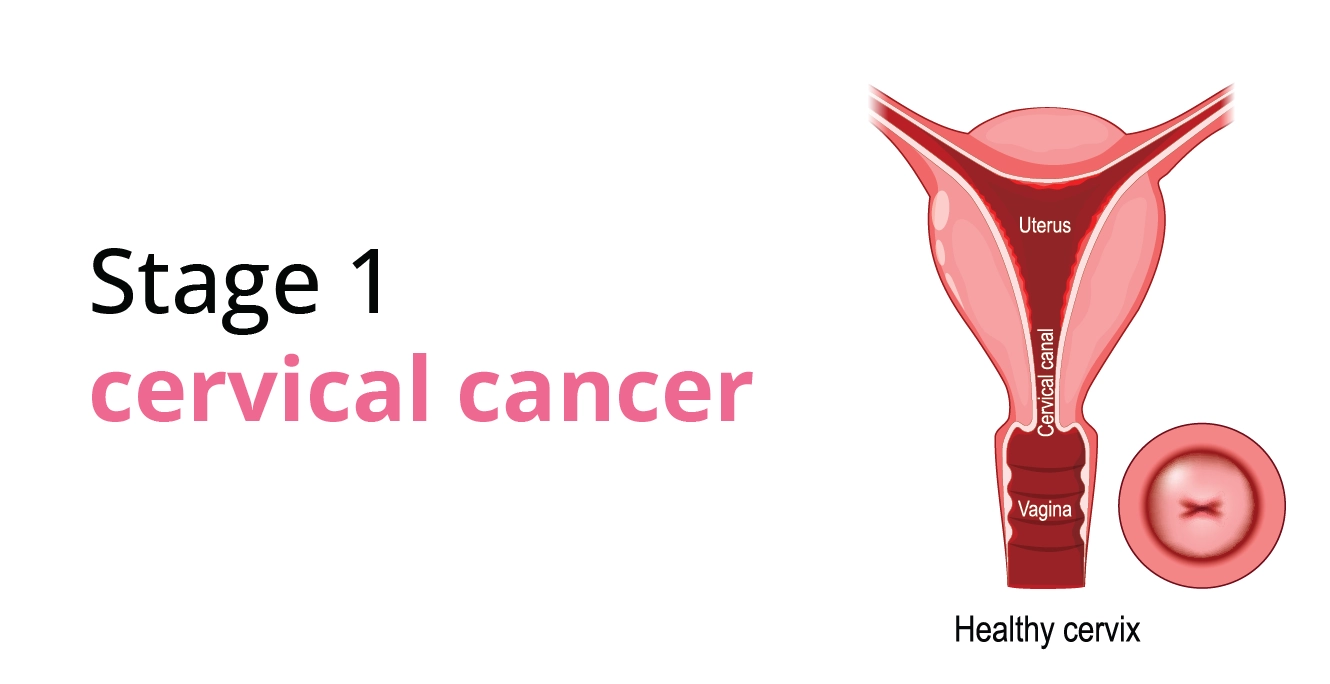
The cervix is the lower part of the uterus that is connected to the vagina. Most of the cases of cervical cancer are related to continuous infection that is caused by human papillomavirus also known as HPV. If the tumour is not detected or treated in precancerous stages, it can progress into higher stages like stage 2.
What is Stage 2 Cervical Cancer?
Stage 2 cervical cancer indicates that cancer has spread beyond the cervix into the surrounding tissues but hasn’t reached the pelvic walls or the lower third of the vagina. It is further classified into two sub-stages
- Stage 2A: Cancer has spread to the upper part of the vagina but has not affected the parametrium (tissue beside the cervix).
- Stage 2B: Cancer has extended into the parametrium involving tissues surrounding the uterus but not beyond.
Keeping a check on the progression of abnormal cell growth especially in stage 2, is important for making the right decisions about treatment procedures.
Symptoms of Stage 2 Cervical Cancer
Recognising symptoms early can improve treatment outcomes. Common signs of stage 2 cervical cancer include:
- Abnormal vaginal bleeding such as bleeding between periods, after intercourse, or post-menopause.
- Abnormal vaginal discharge including watery, bloody or foul-smelling discharge.
- Continuous discomfort or pain in the lower abdomen/pelvic area.
- Dyspareunia i.e. pain during sexual activity.
- Difficulty urinating or increased frequency due to pressure on nearby organs.
Diagnosis of Stage 2 Cervical Cancer
Early diagnosis is vital for effective treatment. The diagnostic process usually includes
| Test Name | Why is it Done? |
| Pap Smear Test | It is done to detect abnormal cells in the cervix. This is often the first step in cervical cancer screening. |
| HPV Test | It helps in identifying the presence of high-risk HPV strains as they are linked to cervical cancer. |
| Colposcopy | This procedure involves a detailed examination of the cervix using a magnifying device to detect abnormal cells. |
| Biopsy | A small tissue sample is taken for microscopic analysis to confirm the cancer and determine the stage. |
| Imaging Tests | MRI, CT scan or ultrasound will help assess the size of the tumour and confirm that it has not spread. |
Treatment for Stage 2 Cervical Cancer
The treatment for stage 2 cervical cancer depends on the sub-stage and overall health of the patient. The most popular treatments are:
| Treatment | Type | Description | Usage in Stage 2 Cervical Cancer | Key Benefits |
| Radiotherapy | External Beam Radiation Therapy (EBRT) | High-energy X-rays target the tumour from outside the body. | Used for both 2A and 2B stages to shrink the tumour and destroy cancer cells. | Non-invasive, precisely targets tumours. |
| Brachytherapy | Internal radiation is delivered directly to the cervix via a device. | Often combined with EBRT to enhance treatment effectiveness. | Delivers higher doses directly to the tumour, sparing nearby tissues. | |
| Chemotherapy | Anti-cancer drugs (e.g., cisplatin) administered intravenously | Used in conjunction with radiotherapy (chemoradiation) to enhance the effects of radiation. | Targets cancer cells throughout the body, and reduces the risk of spread. | |
| Surgery | Radical Hysterectomy | Surgical removal of the uterus, cervix, part of the vagina, and nearby lymph nodes. | Suitable for specific cases in stage 2A where cancer has not spread extensively. | Provides a chance for complete tumour removal in early 2A cases. |
| Targeted Therapy | Bevacizumab | A drug that inhibits the formation of new blood vessels supplying the tumour. | Combined with chemotherapy in advanced cases or when cancer resists initial treatment. | Reduces tumour growth and spread by starving cancer cells of nutrients. |
Is Stage 2 Cervical Cancer Curable?
Yes, stage 2 cervical cancer is curable in many cases, especially with timely and appropriate treatment. According to medical studies, the prognosis improves significantly with a multidisciplinary approach combining radiation and chemotherapy.
Survival Rate of Stage 2 Cervical Cancer
The five-year survival rate for stage 2 cervical cancer is approximately 58–63%, depending on factors like age, overall health, and treatment response. These statistics highlight the importance of early detection and adherence to treatment plans.
High-Risk Factors for Stage 2 Cervical Cancer
Certain groups are more susceptible to developing cervical cancer due to specific risk factors. The following chart highlights these factors and their impact.
| Risk Factor | Description | Why It Increases Risk |
| Persistent HPV Infection | Long-term infection with high-risk types of human papillomavirus (HPV) such as types 16 and 18 | Causes genetic changes in cervical cells, leading to cancer development over time. |
| Weakened Immune System | Conditions like HIV/AIDS or use of immunosuppressive drugs (e.g., after organ transplants). | Reduces the body’s ability to fight HPV infections and abnormal cell growth. |
| Multiple Full-Term Pregnancies | Women with three or more full-term pregnancies. | Hormonal imbalance and cervical trauma increase susceptibility to HPV-related changes. |
| Early Sexual Activity | Sexual intercourse before the age of 16. | Increases lifetime exposure to HPV and cervical cell vulnerability to infections. |
| Multiple Sexual Partners | Having more than one sexual partner or a partner with multiple sexual partners. | Raises the risk of HPV exposure and transmission. |
| Long-Term Use of Oral Contraceptives | Use of birth control pills for more than five years. | Prolonged hormonal exposure may influence cervical cell changes. |
| Family History of Cervical Cancer | Close relatives with a history of cervical cancer. | Indicates a genetic predisposition or shared environmental risk factors. |
Suggestion:
Being aware of the risk factors is important for the prevention of cervical cancer. A few steps that can significantly help are:
✔Regular monitoring
✔HPV vaccination
✔Maintaining a healthy lifestyle
Lifestyle Changes for Managing Stage 2 Cervical Cancer
Medical treatment is important to get the right cure for cervical cancer but some lifestyle changes can complement treatment.
- Healthy Diet: Include fruits, vegetables, whole grains, and lean proteins to boost immunity.
- Exercise: Regular physical activity can improve energy levels and reduce treatment side effects.
- Quit Smoking: Smoking weakens the immune system and may affect treatment outcomes.
- Stress Management: Practices like yoga, meditation or counselling can help manage anxiety during recovery.
Does Stage 2 Cervical Cancer Affect Fertility?
Surgery & radiation therapy commonly used in the treatment of stage 2 cervical cancer can affect fertility. A structured analysis to assess the implications and to navigate the options of fertility preservation for cancer treatment would be beneficial. The following table briefly explains these aspects:
| Aspect | Detail |
| Impact on Fertility | Radiation Therapy:
It can damage ovaries and uterine lining, making pregnancy difficult. Radical Hysterectomy: Removes the uterus, permanently affecting the ability to carry a pregnancy. |
| Fertility Preservation Options | Ovarian Transposition (Oophoropexy):
A surgical procedure that moves ovaries out of the radiation field to protect them from damage. Egg Freezing or Embryo Freezing (Cryopreservation): Eggs or embryos are harvested and frozen before treatment for future use. Fertility-Sparing Surgery (Only in select cases): Certain surgeries preserve the uterus and ovaries depending on the cancer spread. |
| Key Considerations before you opt for any treatment | Type and stage of cancer. Desire for future pregnancies. Time available before treatment begins. Associated risks and success rates of preservation methods. |
| Post-Treatment Options: Alternatives for Parenthood | Surrogacy: Using a gestational carrier with preserved eggs or embryos.
Adoption: An alternative route to parenthood if fertility preservation is not possible. |
Key Notes:
- Fertility preservation discussions should occur before starting treatment.
- Collaborating with a fertility specialist and oncologist ensures the best-personalised plan.
- Emotional counselling can support decision-making during this challenging period.
Word From An Expert
“Stage 2 cervical cancer is a serious but manageable condition with advancements in medical science. Recognising the symptoms, seeking timely diagnosis, and adhering to treatment can significantly improve outcomes. Supportive lifestyle changes and open communication with healthcare professionals can help women navigate this challenging journey with strength and hope”.~ Dr. Madhulika Singh
Our Fertility Specialists
Related Blogs
To know more
Birla Fertility & IVF aims at transforming the future of fertility globally, through outstanding clinical outcomes, research, innovation and compassionate care.
Had an IVF Failure?
Talk to our fertility experts

 Our Centers
Our Centers